BY LINCOLN ANDERSON | Downtowners now have a powerful new ally on their side in the fight against breast cancer: The outpatient imaging center at Lenox Health Greenwich Village.
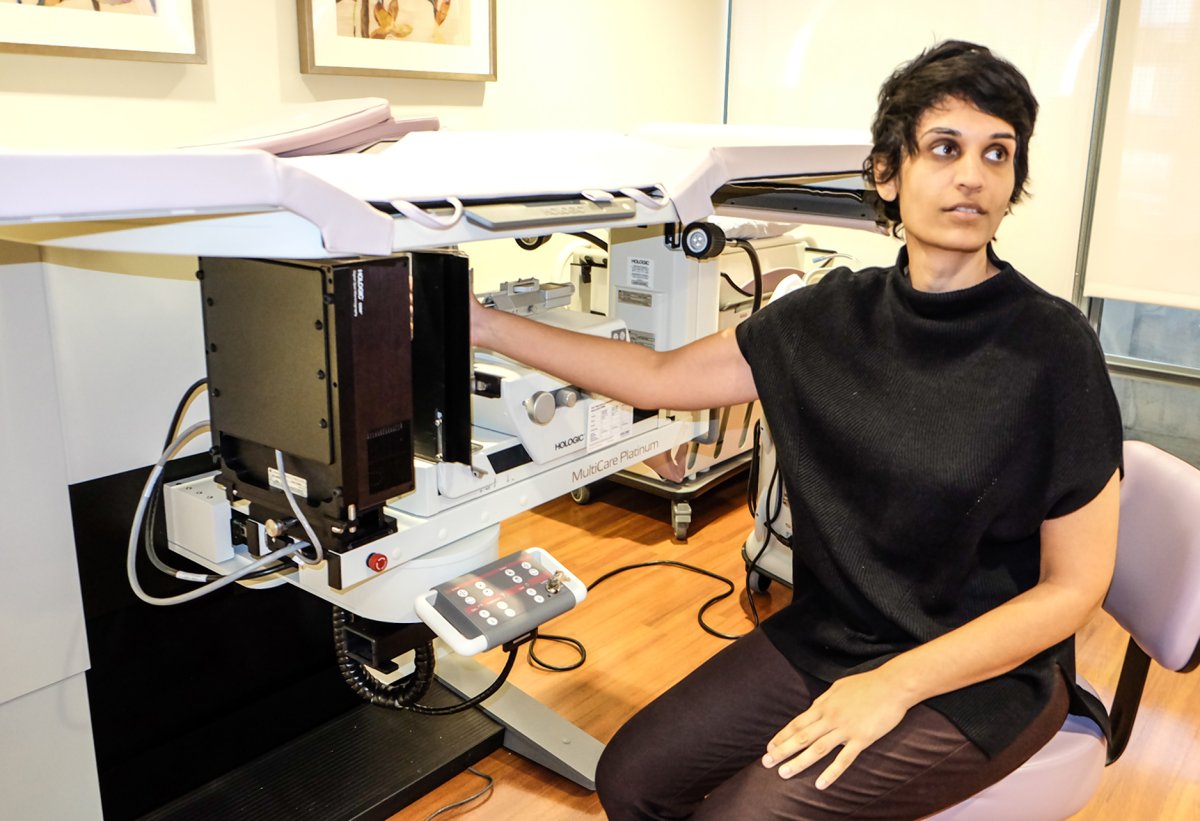
More to the point, they have Dr. Kavita Patel, the center’s medical director, whose training was specifically in breast imaging.
The imaging center — which is an extension of Lenox Hill Hospital — opened this July on the third floor of Northwell’s new comprehensive care center, at W. 13th St. and Seventh Ave. The building’s first floor opened one year earlier as a stand-alone emergency department.
As far as breast-imaging services, the heart of the new center is its state-of-the-art tomosynthesis mammogram machine.
Annual mammograms are the only screening test proven to reduce the risk of dying from breast cancer. Starting screenings at age 40 saves significantly more lives and adds more years of life for survivors than delaying screening until age 45 or 50.
As opposed to old-school mammograms, tomosynthesis, which was approved by the F.D.A. in 2008, represents a quantum leap forward. The older machines would only X-ray the breast in two dimensions — so it was much harder to distinguish different tissues and identify problems if they were there. Tomosynthesis, on the other hand, takes many “slices” of the breast, both vertically and horizontally, giving an exponentially more accurate picture of what is going on.
As Patel explained, there are actually four different types of breast density, ranging from fatty to extremely dense. Having dense breast tissue may increase the chance of getting cancer. (Under a new New York State law, signed into effect by Governor Andrew Cuomo, women’s mammogram results must now also include one of four letters indicating their type of breast density.)
Dense breasts also make it harder to detect the disease in both self-exams and traditional mammograms. Tomosynthesis, though has changed the equation.
“We are now ‘slicing’ instead of going just on top,” Patel explained of the revolutionary diagnostic tool. “This has made a significant, significant difference. It’s increasing the cancer detection rate by 20 to 30 percent.”

There were initially concerns about increased radiation from tomosynthesis. But according to Patel, due to improved technology, the dose doled out by the machines is now no greater than 2D mammograms.
“This is a huge breakthrough,” she said.
The dose is equal to “a few weeks of natural background radiation,” according to a fact sheet on breast cancer screening exams that Patel provided.
Not only is the new screening method more likely to help detect cancer early, it also reduces the number of “false positives,” so that people don’t have to come back for needless follow-up tests and procedures.
“Part of the problem with traditional mammograms is we were finding stuff that wasn’t real,” the doctor explained. “We were then doing ultrasound and biopsies.”
According to Patel, regarding breast health, the imaging center is seeing mostly patients for annual screenings. A small percentage of these are called back for additional views or ultrasound. A still smaller percentage have biopsies performed. An even smaller number are diagnosed with cancer. This reflects national averages. For every 1,000 women screened, 100 will return for an additional mammogram or ultrasound. Sixty-one of these will require additional viewing and be found to have nothing wrong. Twenty others will find that what was seen is not likely cancer and return in six months to keep an eye on the finding. Nineteen will have a minimally invasive biopsy. Five out of the original 1,000 women will be diagnosed with breast cancer.
Regarding biopsies, Patel performs them herself. Another room has what is known as a stereotactic surgical setup. It includes a table with a hole in it. The patient lies down on her stomach and her breast goes through the hole where it is held in a vise-like device and X-rayed. The image is then viewed on a screen, guiding Patel as she inserts a needle right into the suspect spot and extracts a bit of tissue. This is known as a percutaneous, or “through the skin,” biopsy and has been the “standard of care” over the past 10 years, Patel noted. Again, it’s an advance over older-style biopsies, which were more traumatic and left larger scars.
Mammograms are covered under the Affordable Care Act.
Again, the single most important thing a woman can do in terms of breast health is to get a mammogram, preferably tomosynthesis, once a year, Patel said. Personal breast exams should be done as often as once a month, she said.
As far as nutrition and its impact on breast health, Patel said caffeine can have an effect.
“Caffeine can be a culprit in breast cysts — which are bags of water,” she noted, though adding that these are not cancerous.
Obesity is also a risk factor, she noted, likely due to the increased estrogen it produces.
Men can get breast cancer, too, but it’s extremely rare. Although the center has screened some men, she said, “It makes up a fraction of what we do.”
If a man has breast cancer, though, women in his family are at higher risk, but the same doesn’t hold true vice versa, Patel said.
Asked about whether genetic testing would ever be advisable, Patel said it could be considered if a first-degree relative — a mother, sister or first cousin — had breast cancer very young.
The L.H.G.V. imaging center does about 15 to 20 mammograms per day. Each takes only a few minutes. Currently, because the still-new facility is not seeing patients at full capacity, people can conveniently get a same-day appointment. The results are also fast.
“Part of the benefit here is that we will read the studies on-site,” she said.
The imaging center is open Monday to Friday, from 7 a.m. to 7 p.m., and Saturday, from 8 a.m. to 4 p.m.
Asked what else women can do to ensure breast health, she offered some tried-and-true advice: “A balanced diet and exercise.”

Patel aims to make the W. 13th St. facility Downtown’s best, in terms of breast imaging. Northwell, the center’s parent health company, is currently doing outreach to women from Harlem to the Battery.
A native Staten Islander, Patel still lives there, but really enjoys her new workplace’s location — from its people to its cuisine — plus the brand-new L.H.G.V. medical facility, located in the former National Maritime Union building, the top floors of which are currently being gut-renovated for surgical suites and physicians’ offices.
“I love working in this neighborhood,” she said. “I feel like I’m in the best neighborhood in Manhattan. I have a fantastic lunch every day. The people are so friendly. And it’s great to help fill the gap left behind in the closure of St. Vincent’s. And we’re happy to take care of the community here.
“It is my desire and our goal to become an integrated part of the community,” Patel said. “I am passionate about breast imaging, and I want to build a top-notch facility here for Downtown and Lower Manhattan.”